Chapter 48
The Immune system
The functions of the immune system
- Provides defense against pathogens
- Pathogens are disease causing organisms
- Prokaryotes and eukaryotes
- Defense against cancer by recognizing and eliminating grossly abnormal cells: immune surveilance
Cells of the immune system
- Leukoctyes - general term for the cells of the immune system
- White blood cells
- Derived from a common precursor in the bone marrow
- Circulate in the blood and lymphatic fluids to tissues all around the body
- Granulocytes
- Contain visible granules in their cytoplasm
- Secrete chemicals that attack pathogens or that change the behavior of host tissues near a site of infection
- Includes basophils, mast cells
- Also includes eosinophils and neutrophils, which are also phagocytic
- Phagocytes
- Phagocytose foreign marterial or debris from dead infected cells
- Includes macrophages, monocytes, basophils, and dendritic cells
- Neutrophils and eosinophils are also phagocytic, but technically eosinophils
- Technically granulocytes if you categorize based on appearance, but highly phagocytotic
- Lymphocytes
- Recognize specific pathogens or cells that have been infected by a pathogen
- Includes B cells, T cells, and NK cells
The immune system
Innate immunity
- First line of defense
- Anatomical barriers (e.g. epithelial coverings)
- Physiological barriers (e.g. secretions)
- Promotion of non-pathogenic microbes
- Second line of defense
- Granulocytes, phagocytes, and NK cells
- Inflammatory response
- Complement system
- A series of proteins secreted the liver that circulate in the blood and lymphatic fluid and get activated by the signals that lymphocytes secrete near sites of infection
- Not specific to the type of infection
Adaptive (acquired) immunity
- Third line of defense
- More targeted, more specific
- B cells produce and secrete antibodies that target extracellular pathogens
- Cytotoxic T cells target and kill infected cells to limit the ability of pathogens to reproduce
- Helper T cells are necessary for the activation of the cells above
There is lots of cross over between the two "divisions" of the immune system, including NK cells and dendritic cells. NK cells and dendritic cells are technically part of the adaptive immune system because they activate B cells and T cells, but they work with the innate immune system to help determine what B cells and T cells to activate.
Innate immune system
Always on, but very generic.
Components of the innate immune system
First line of defense
-
Anatomical, physiological, structural aspects of tissues that act as a barrier to infection
- Tissues in our body that are exposed to the environment are all epithelial tissues
- Epithelial tissues are composed of lots of cells packed closely together with tight cell-cell contact, tight junctions, gap junctions, desmosomes, etc sitting on the basal lamina
- These are multi-layered
- The epidermis is a multi-layered epithelium.
- All the outermost cells are dead in skin
- This is why we are constantly shedding
- A virus can't infect a dead cell, therefore, this helps as a barrier to infection
- Epithelial tissues are composed of lots of cells packed closely together with tight cell-cell contact, tight junctions, gap junctions, desmosomes, etc sitting on the basal lamina
- Physiological barriers to infection include different secretions that are secreted by epithelial tissues that make the environment unfavorable to any pathogens that might be nearby
- Mucus traps any potential pathogens before they reach tissue, and this mucus is either expelled from the body or degraded in the digestive system
- Tears include lysozyme, an antibacterial enzyme
- The nasal passages are lined with mucous secretions and hairs that trap pathogens
- The digestive tract helps dispose of pathogens that are trapped in saliva and mucus and then swallowed. Most are destroyed by the low pH of the stomach.
Second line of defense
- Mast cells are a type of granulocyte that cause more blood to be delivered to the site of infection
- Macrophages are very good at recognizing bacterial and viruses in the environment and then phagocytosing those bacteria and viruses
- Neutrophils will attack pathogens both inside and outside the cell
- The inflammatory response is one way these innate immune cells work together in response to infection
- Platelets try to clot to seal cuts in the skin, which are activated via exposure to the air
- If pathogens sneak in before the clotting process finishes, they are in an environment that is attractive to immune cells, which secrete more chemicals that attract more immune cells
- These cells attack the pathogens
- Mast cells secrete histamine
- Cause nearby blood vessels to dilate and become more permeable
- How do the phagocytic leukocytes carry out phagocytosis
- The bacterium is attached to the membrane evaginations called psudopdia
- Bacterium is ingested, forming phagosome
- Phagosome fuses with lysosome
- Bacterium is killed and then digested by lysosomal enzymes
- Low pH and hydrolases from the lysosome are used
- Digestion products are released from cell
- How do phagocytic leukocytes recognize bacteria and viruses?
- PAMPs = Pathogen-Associated Molecular Patterns = molecules found on broad categories of pathogens and that are recognized by cells of the innate immune system
- Bacterial PAMPs include components of bacterial cell walls (e.g. peptidoglyan), bacterial cell membranes (e.g. lipopolysaccharide) or bacterial proteins (e.g. flagellin)
- Viral PAMPs include dsRNA and some capsid proteins
- PRRs = Pattern Recognition Receptors = classes of receptors found on innate immune cells and that recognize a particular category of PAMP.
- Example: Toll-like receptors (TLRs)
- PAMPs = Pathogen-Associated Molecular Patterns = molecules found on broad categories of pathogens and that are recognized by cells of the innate immune system
- Activation of the complement system
- Composed of about 30 different proteins (most secreted by cells of the liver) that circulate in the blood and are activated in specific regions in response to signals from the innate or adaptive immune cells that have encountered pathogens
- When activated, the complement system proteins:
- promote more efficient phagocytosis of viruses or bacteria by phagocytes
- trigger an inflammatory response by attracting neutrophils and macrophages to the area
- form pores in the cell walls of bacteria, rupturing them
Adaptive Immune System
- Slower and takes a while to get activated, but much more specific and robust
- Subclass of lymphocytes that include B-cells and categories of T-cells
- These become activated in response to exposure to a specific pathogen
- Born in bone marrow
- Stem cells in the bone marrow make them
- Born in bone marrow
- Precursors to B-cells mature in the bone marrow then are released, while precursors to T-cells mature in the thymus
- Lymphatic system is where these circulate most
- They also circulate in the blood
- These become activated in response to exposure to a specific pathogen
- Antigen and immunogen are used interchangeably, but are not technically the same thing
- Antigen will be used exclusively for the rest of the chapter
- B-cells and cytotoxic T-cells represent two branches of the adaptive immune response
- B-cells secrete antibodies that bind to extracellular antigens in the humoral response
- Cytotoxic T-cells recognize and kill infected cells that display antigens from the pathogen on the cell surface through the cell-mediated response
- B-cells and T-cells recognize specific antigens through receptors on the surface that go with B-cell receptors and T-cell receptors
- The B-cell receptor has 2 identical arms
- The T-cell receptor has 1 arm
- Both are anchored in the cell membrane
- Both are proteins composed of different subunits
- B-cell receptors have light and heavy chains
- T-cell receptors have an alpha and a beta chain, each encoded by a different gene
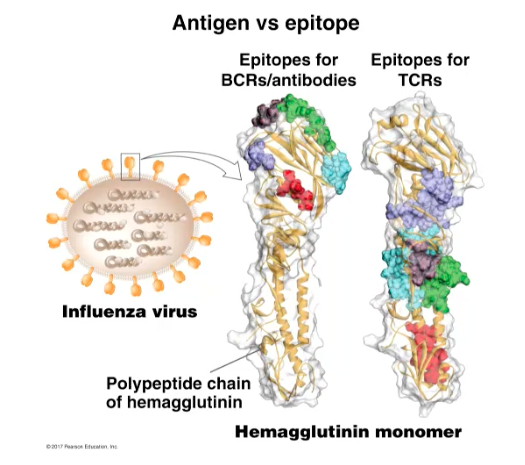
- A molecule that binds to a T-cell receptor or a B-cell receptor is an antigen. The specific site on the antigen where that receptor is bound is called the epitope.
- The regions on the receptors that are the same are called the constant regions
- Each type of B-cell makes a specific B-cell receptor that will recognize one specific epitope
- Each T-cell makes one specific T-cell receptor that will recognize one specific epitope
- This is possible through DNA recombination
- Not the same as DNA recombination in meiosis
- Occurs during embryonic development of the B-cell and T-cell precursors
- This is possible through DNA recombination
- B-cells end up with different versions of the BCR with different epitope specificities
- Light-chain DNA
- Variable segments (40 different segments)
- Joining segments (5 different segments)
- Constant segment
- Heavy-chain DNA
- Variable segments (51 segments)
- Diversity segments (27 segments)
- Joining segments (6 segments)
- Constant segment
- When an individual B-cell is developing, its going to remove all but 1 variable and joining segment from the light-chain DNA and all but 1 variable, diversity, and joining segment from the heavy-chain DNA. This process is different in every developed B-cell.
- As the B-cell precursor is in the embryo, DNA recombination is occuring and the above occurs
- 40 x 5 = 200 different light chain genes are possible
- 51 x 7 x 6 = 8262 different heavy chains are possible
- 200 x 8262 = 1.65x10^6 different versions of the BCR are possible
- Each B-cell only makes one receptor type, but in the population, this is how many are possible
- This process has already happened in embryonic development
- Each one is potentially able to recognize a different antigen
- Light-chain DNA
- When a B-cell or T-cell encounters an antigen that it recognizes, it undergoes clonal expansion and selection. This is where the B-cell or T-cell has rapid mitotic divisions to create more to fight the pathogen. Then, they have a series of cellular divisions that allow them to properly attack the pathogen. In B-cells, this is when they get ready to secrete more hormones, and T-cells get ready to identify and kill infected cells.
- Clonal expansion and selection
- Lymphocytes proliferate rapidly when they encounter an antigen they recognize
- The B-cell has the antigen bind to a receptor, then it starts a signaling cascade and the activated lymphocytes are cloned
- B-cells have a lot more rough ER after being activated
- The process of lymphocyte activation is occurring in the peripheral lymphoid tissues, in the lymphatic vessels, in the lymph nodes, and in tissues associated with the lymphatic system
- This occurs after DNA recombination
- Lymphocyte activation
- Initial exposure to the antigen partially activates the B-cell or the T-cell
- T-cells: phagocytic cells "present" antigen they have internalized to T-cells
- B-cells: encounter the antigen directly, usually in the lymph nodes or vessels
- The partially-activated B-cell or T_c-cell receive signals called cytokines from T_h-cells that have been activated by the same antigen
- This is kind of a safety check to help limit the likelihood of the accidental activation
- Initial exposure to the antigen partially activates the B-cell or the T-cell
- MHC complexes are membrane proteins that display potential antigens on the cell surface
- T-cell activation
- T_h (CD4^+) and T_c (CD8^+) cells first recognize class II MHC-presented antigens, triggering clonal expansion
- The activated T_H cells then secrete cytokines to help fully activate the cytotoxic T-cells if (T_h 1) or B-cells (if T_h 2)
- The activated T_c cells then leave the lymph system and enter the blood, looking for infected cells displaying the same antigen on MHC class I.
- B-cell activation
- B-cell encounters the appropriate antigen, phagocytoses it, and displays fragments on surface via MHC class II.
- B-cell presents the antigen to a helped T-cell specific for that antigen, activating it
- Activated helper T-cell (T_H 2) then secretes cytokines that complete the activation of the B-cell
- Clonal expansions, antibody production
- Culmination - fully activated B-cells or T_c-cells mount a response against infection
- Culmination in B-cells
- Antibodies are basically secreted versions of the BCR